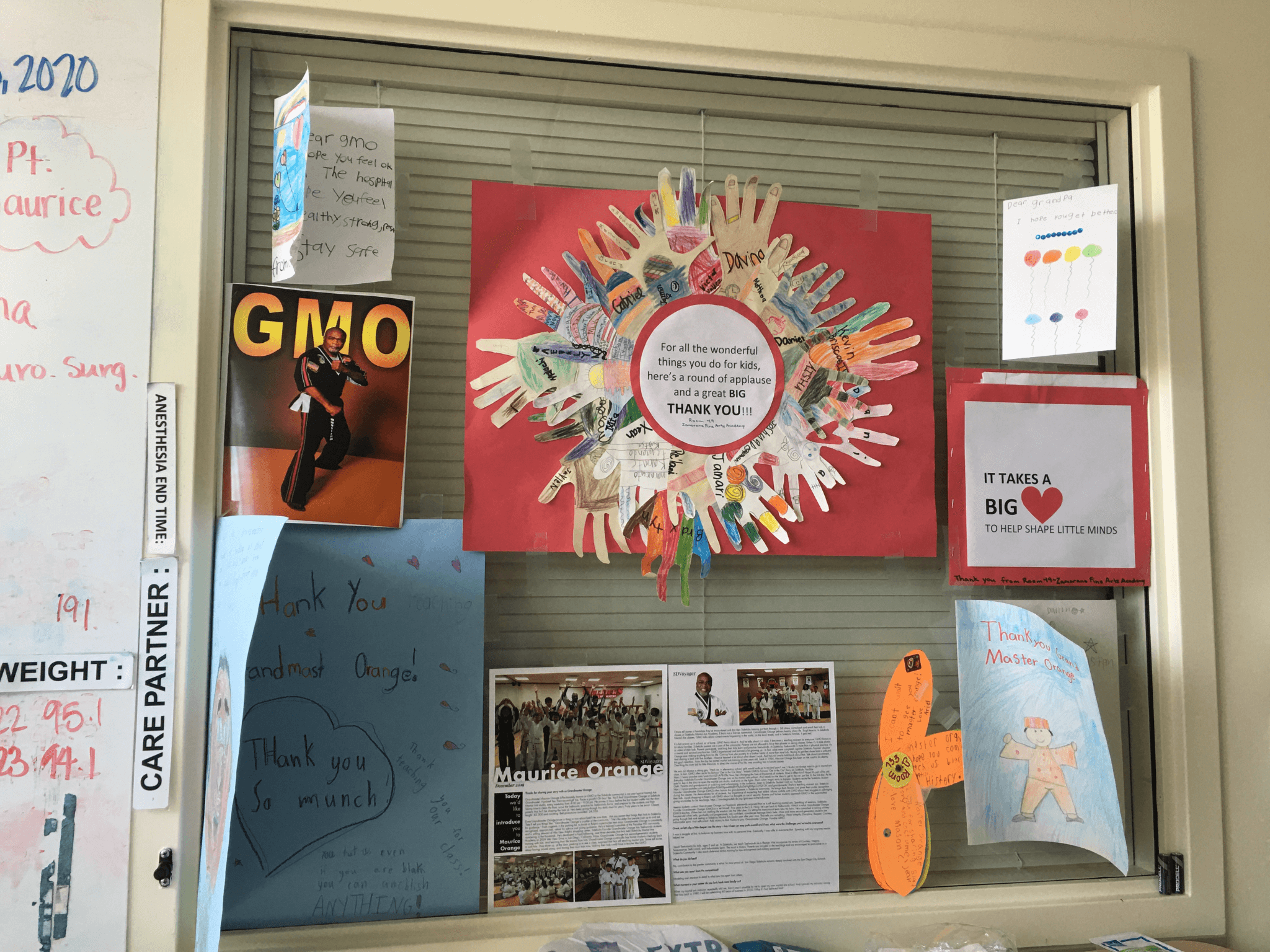
Near Death on Sunday, August 16, 2020
Dr. Diane Wintz called me from Sharp Memorial Intensive Care Unit. She had taken over treating my fiancé after his near-death motorcycle accident on Friday, August 14, 2020. He had to be treated aggressively due to 36 documented injuries. He had a breathing tube and was on a ventilator; had a right-sided chest tube between the right lung and the chest wall, to evacuate air because the lung had a puncture. That was a minor injury, she said.
My love had received a blood and plasma transfusion. He had low blood pressure and signs of (internal) bleeding. They did a CAT scan due to the nature of his (brain) injuries. Which were: #1. Subarachnoid hemorrhage. According to my furious notes, she explained this injury as being on the outside area of the brain, sloshing around, not pushing on the brain. #2. Diffuse Axonal injury, or D.A.I. which based on the CAT scan she thinks it may be. Dr. Wintz. helped me envision this by thinking of a perfect Jell-O mold (i.e. the brain before injury) and travelling in a car, the Jell-O mold gets shaken up, resulting in tears and things like that happening to it. There are little tears in the brain matter itself, was the point she made clear to me.
Unpredictable Recovery
Then she went on to tell me that these injuries are unpredictable in terms of recovery. In my notes from that day, I wrote: “Unpredictable in terms of recovery. Death related to this injury. Some degree of recovery. She cannot (?) how he will recover.”
Back to the list of injuries. #3 Injury to blood vessels that go up to the brain. Blood vessels injured on the left side that go to the brain. May be a stroke, high risk. Aspirin would be critical to help prevent a stroke. However, they cannot give aspirin due to the bleeding.
This is the reason why fixing the left wrist was so important, Dr. Wintz. explained. Because if he had a stroke on the left side (of the brain), it would affect the right side of his body. He will be dependent on the left. (In retrospect he really would have been screwed if a stroke had occurred. Because he ended up having the left arm amputated below the elbow.) He had already undergone surgery on Saturday, August 15, due to the critical nature of his numerous bodily injuries.
On with the injuries: #4 Pelvis injured. (It was documented as an open-book pelvic fracture.) My notes say, “Legs straddled. Legs very, very straddled.” (I think that was how he was ejected from the bike.) “Pelvis circle, pubic bone hit and opened at the bone. Bleeding at pelvic injury fixed the night he came in. Bleeding stopped.”
Watching and Waiting
At this point, watching and waiting for brain swelling to stabilize before we do anything moving forward. Figure out his mental status. Need to determine, if he had a stoke? Can he move? They have him on sedation and pain medication. Keep sedated so brain pressure does not go up. Next step is to pull the medication. Can have a lot of pain and discomfort.
As if I wasn’t scared enough, she told me that. “Survival does not tell anything about function in life.” My harrowing notes read: Don’t want to do everything (to keep him alive) and (have him) be vegetative. And have to live at a facility. Now is not the time for making decisions. Keeping him alive and safe right now. There will be decisions to be made out of function. His doctors on Tuesday and Wednesday would be taking over from her.
Breathing tube would be uncomfortable (without having him sedated) so they could not get an accurate read on him. Tuesday (the plan is) to move it to tracheostomy. See where we are. Remove sedation medication. She made a point to be clear that death can happen in hospitals. The brain is needed to run the liver, and intestines. If his brain gets very swollen, he can… (I could not even write the word.)
Threat to Life
“Think about it,” she told me. It’s not an issue now. Expects it will be. Another analogy she gave me, it’s like when you bump your knee on a table. It hurts and then the hurt goes away. Bruising or swelling occurs days later. His brain pressure number was high. They were trying to get it down.
As if all that wasn’t bad enough, she added that people with brain injuries on breathing machines have a very high risk of pneumonia. She emphasized that it was a threat to life. Threat to life… The words echoed inside my head.
Still at a place where as healthy as he was pre-injury. Doing everything to keep him alive. She told me, “He’s not going to be the same. Even with perfect recovery. He will not be perfect in life. Not like he was before.”
“Be hopeful. Be realistic. There’s no decision to be made right now. We’re watching and waiting. Providing supportive care.” She reiterated.
Just the Beginning
Dr. Wintz continued on. My fiancé had a blood clot right behind the trachea. Not stable. Still very near death. Waiting and watching his brain pressure. “As we get further in time and he’s still alive,” she said, “the more encouraging it becomes.” My heart jumped out of my chest and grabbed onto the pen; my hopeful notes emphasized:
* Good note is Stability. *
* Brain pressure normal range today. *
“It’s our job to communicate realistic expectations,” Dr. Wintz told me. “We are giving him real aggressive treatment, and seeing improvement…”
Shocked and stung, I hung up the phone in a daze. My best friend, who had been standing in the hallway listening, said, “Oh my god Cher, that was gnarly.”
And that was just the beginning.